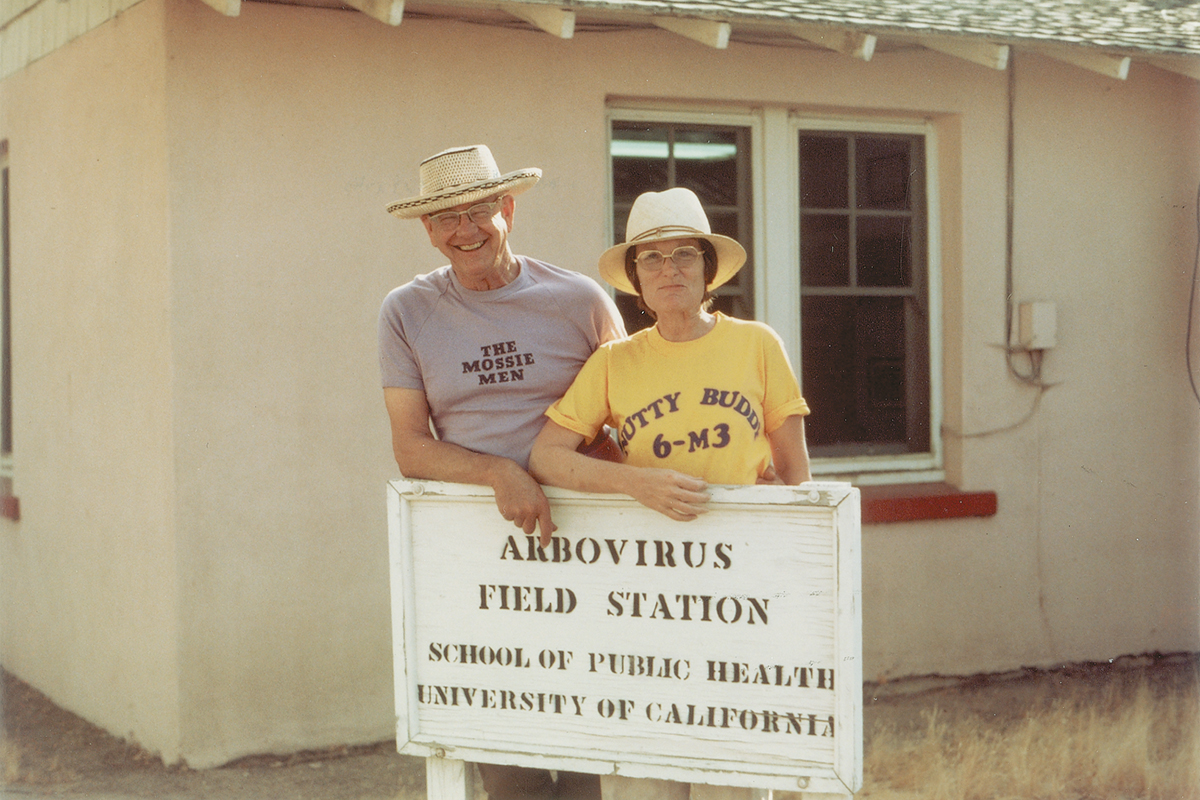
 William C. Reeves, professor of epidemiology and giant in the field of arbovirology stands with biostatistician and researcher Marilyn Milby at the School’s Arbovirus Field Station in Bakersfield, Calif.
William C. Reeves, professor of epidemiology and giant in the field of arbovirology stands with biostatistician and researcher Marilyn Milby at the School’s Arbovirus Field Station in Bakersfield, Calif.
The deadliest animal in the world is a miniscule flying insect that carries disease.
Mosquitoes, which to many of us in the United States aren’t much more than a backyard nuisance, transmit viruses like yellow fever, dengue, Zika, and chikungunya. These viruses can lead to symptoms like rash, vomiting, headaches, and even birth defects like microcephaly. Too often, they result in death. The World Health Organization estimates that mosquitoes account for the premature death of 720,000 people around the world each year.
The field of arthropod-borne virology, or arbovirology, aims to tackle this global problem. “By definition of vector-borne diseases, you have to look at much beyond just the biology,” says Eva Harris, molecular biologist and professor at the School of Public Health. “You have your human aspect, and you have your viral aspect, but you also have your mosquito aspect.”
Entomologists must think like epidemiologists, statisticians like ecologists, biologists like sociologists, and so on. This transdisciplinary approach defined the career of the late William C. Reeves, the UC Berkeley professor of epidemiology often credited for coining the term “arbovirus.” A trained entomologist, Reeves established a legacy in the field of public health of groundbreaking research and work in the field to combat mosquito-borne illness.
From Harris, who looks at the pathology of viruses and the populations they affect, to John Marshall, a biostatistician at the frontlines of mosquito genetics research, today’s School of Public Health faculty members continue that legacy established by Reeves, who would often tell his students and colleagues that to survey and control a mosquito, you must think like one.
Arbovirology in the making
Yellow fever and dengue had already caused widespread sickness and death for centuries before scientists identified arthropods as the vehicle for transmission. In 1881, a Cuban physician named Carlos Finlay presented his mosquito-as-vector theory to the International Sanitation Conference. Yellow fever periodically ravaged Havana, and Finlay aimed to find out why. He pointed to Aedes aegypti—the species of mosquito that would come to be known as the “yellow fever mosquito,” though this species would later prove capable of transmitting dengue, chikungunya, and Zika as well.
Fifty-five years later, a tall, broad-shouldered 20-year-old from rural Southern California walked onto the UC Berkeley campus as a student for the first time.
Bill Reeves wasn’t particularly studious then. At the end of his career, he would tell science historian Sally Smith Hughes that he delegated much of his growing-up years playing basketball or catching insects. “I wasn’t a student,” he said. “I was too interested in chasing bugs in my spare time.”

William C. Reeves and Australian researcher Malcolm Simpson collect mosquitoes from pools of standing water in Murray Valley, Australia, 1952.
Reeves came to Berkeley to study entomology and the School of Public Health had not yet been established. But either way the field of public health hadn’t yet crossed Reeves’s mind. He bounced from courses and field work in forest entomology to agricultural and economic entomology, all while bumping elbows on the intramural basketball court with other aspiring bug scientists.
Fate intervened. A serious knee injury ended his basketball days and confined him to his textbooks. He leaned heavily into his academic interests until he had taken every entomology course offered on campus, plus courses in microbiology and parasitology. When he transitioned into the entomology graduate program, a professor named W.B. Herms, who had done research on tick-borne diseases in California, offered Reeves a job.
Reeves recalled that this job paid $45 a month, “enough to live on,” though he “never had a pay raise.” He accepted and became a full-time teaching assistant in medical entomology—a position that further steeped him in the biology of both mosquitoes and the potential diseases they carry.
At that time, thousands of horses across the western United States had died from a virus known as western equine encephalitis. There was no known cause of transmission, though UC Berkeley pathologist Karl F. Meyer had hypothesized that mosquitoes had something to do with it. For his dissertation, Reeves transmitted an isolated strand of the virus to guinea pigs through mosquitoes, proving Meyer’s theory. The discovery enabled public health officials to effectively target a key source of disease transmission, leading to the ability to better control the widespread outbreaks encompassing western North America in the 1940s.
When Reeves earned his PhD, there was still much to be learned about viruses. UC Berkeley offered no course strictly on virology. But Reeves knew one truth about a virus that would set him up to become a pioneer in an emerging field: “It was some little thing that you couldn’t see, you couldn’t smell,” he said. “But it was there, and it was infectious.”
From Bench Science to Public Health
As an entomologist with a PhD, Reeves set a precedent for applying science to the emerging field of public health. In 1943—the same year Reeves graduated—Governor of California Earl Warren signed legislation establishing the School of Public Health. Also in 1943, an epidemic broke out on American soil, in the territory of Hawaii on the edge of World War II. Aedes aegypti delivered dengue to Pearl Harbor.
Reeves got the call to serve, not as a military man but as an epidemiologist. The army had a vested interest in hiring entomologists to control insect-borne diseases among troops. Reeves knew mosquitoes, as well as how to survey and control the diseases they spread. He spent the remainder of the war as a civilian advisor to the military, eventually joining the Armed Forces Epidemiological Board. He returned to Berkeley in 1949 to teach, but not as an entomologist. He joined the new School of Public Health as a professor of epidemiology, a position he held for over 40 years. He also served, albeit reluctantly, for a few years as the School’s fourth dean.
Throughout his career, Reeves’s work at the intersection of entomology and epidemiology provided a cornerstone for applied science in the field of public health. He officially retired in 1987, although he continued to come to the School three or four days a week until the early 2000s—passing along his infectious spirit and drive to others at the School, particularly fellow arbovirologists.

Eva Harris as an associate professor in her lab on the UC Berkeley campus in the early 2000s.
“I always had this drive that I wanted to use science in the real world,” says Eva Harris, thinking back on her time as a Harvard biochemistry student in the 1980s. In those days, she recalls, physicians were the ones who traveled to the communities affected by arthropod-borne and infectious diseases. Bench scientists typically stayed in the lab. It wasn’t yet clear to Harris how to bridge that gap.
Today, Harris is a professor of Infectious Diseases and Vaccinology and director of the Center for Global Public Health. She first made the jump from bench science to public health in Nicaragua, where as a graduate student she was exposed to dengue, literally and figuratively. “I didn’t know what it was,” she says. “I didn’t how how to spell it. I didn’t know it was a virus. But I knew it was a big public health problem.”
Harris has spent much of her 20-year career at Berkeley finding out everything there is to know about dengue. At any given moment, she has multiple active research projects concerning the various aspects of dengue, from its microbiology to the social implications of its spread in certain populations. She calls this a “renaissance approach” to disease surveillance. The science of each virus is a spectrum, she says. Her lab constitutes researchers from various academic backgrounds, from molecular virologists with a knack for primers and assays to epidemiologists with a lens on the sociopolitical aspects of arboviruses.
In 2015, Harris’s transdisciplinary lab pivoted from dengue to Zika following the outbreak and epidemic that originated in Brazil. “When Zika came along, there wasn’t just one question,” says Harris. “There was what I like to call the zillion Zika questions.”
Within a few months, she had projects on the ground that would go on to explain multiple aspects of the virus, such as how it affects a developing fetus and just how many people in Nicaragua were eventually infected.
As Harris continues to find out new things about arboviruses, she works within communities in Nicaragua and elsewhere. Solutions to health problems, she explains, don’t come only from the mind of a microbiologist. Testing for antibody-dependent enhancement in dengue is one thing. Developing a plan to reuse old tires, where standing water collects and mosquitoes breed, is another. “If you do all this work across the whole transdisciplinary approach,” she says, “then you can really see the whole disease.”
Technology on the Virology Tool Belt
John Marshall, like Harris and Reeves, comes from a hard-science background. As an undergraduate in New Zealand, he studied laser physics and molecular biology. He eventually earned a PhD in mathematics from UCLA. “When you do applied mathematics, you can apply it to high-energy physics, or hedge funds if you want to, or climate change,” he says. “Or to any number of diseases and epidemics.”
An assistant professor of Biostatistics, Marshall applies his expertise in mathematics and biostatistics to the latter problem. More specifically, he works to control mosquito-borne diseases by targeting the mosquitoes themselves—by modifying their genetics.
Many people have become more familiar with the CRISPR-Cas9 method. Developed over the last decade by Jennifer Doudna, a biochemist at UC Berkeley, CRISPR marks a significant—some say, revolutionary—step in genome editing technology. Marshall says that CRISPR turns “a haphazard, random process” into “a precise, almost digital process.” Across campus from Doudna, he researches the application of this and other gene-editing technologies to mosquitoes, in order to control the diseases they spread. Specifically, Marshall models strategies for the safe use of genetically modified mosquitoes such that they can be released, shown to be effective, and removed from a population at the end of a trial.

Assistant Professor John Marshall in his Lab in Berkeley Way West in 2018.
As a graduate student at UCLA, Marshall worked with ecologist Charles Taylor, who introduced him to the idea that gene editing in mosquitoes could provide a solution to widescale disease transmission. This research can take a number of approaches. One method involves releasing genetically modified, sterile mosquitoes into a population of disease-carrying mosquitoes. This reduces the number of offspring they have, thereby suppressing the population and disease transmission. Another method involves driving genes into the mosquito population that disrupt their ability to transmit disease—a process made much easier by technology like CRISPR.
Marshall spent a year in Mali talking with people, gauging interest in the use of genetically modified mosquitoes to limit disease and co-organizing biosafety workshops to lead the way to a regulatory framework for releasing these mosquitoes in a responsible way. In that time, Marshall recognized that many Malians were receptive to this technological approach, if it meant saving lives.
“At the time I was doing my PhD, two children were dying every minute in sub-Saharan Africa from malaria,” says Marshall. “Now it’s one child every minute, as a result of bed nets and antimalarial drugs.”
With nearly a billion people in sub-Saharan Africa, the distribution of mosquito nets and medicine goes only so far, says Marshall. Gene editing technology like CRISPR has the potential to finish the job in combination with these other tools.
Gene editing technology comes at the end of a long line of technical advancement in the field of arbovirology. Reeves himself developed techniques to survey mosquitoes, including using carbon dioxide and light to trap them and marking them with a fluorescent dust to track them.
Throughout Harris’s career, she has dealt with much of the lab technology that makes studying arboviruses possible. As a graduate student, she began organizing workshops in Nicaragua to introduce scientists to polymerase chain reaction—a technique of amplifying and replicating DNA, often referred to as “molecular photocopying.” At that time, notes Harris, Nicaragua had little running water and intermittent electricity, but that didn’t stop the advent of technology that has since become ubiquitous in diagnostics and identifying arboviruses. “Polymerase chain reaction is actually quite simple in concept,” says Harris. “And very powerful.”
In 2004, after six decades at the forefront of arbovirology, Reeves passed away at the age of 87. His background “chasing bugs” had led him to become a “giant in his field,” as then Dean Stephen Shortell observed at the time of Reeves’s passing. His methodology for colonizing, controlling, and surveying mosquitoes remained integral throughout the rest of the twentieth century. In fact, just a few years before he died, a dead crow in New York City signaled the start of the West Nile Virus epidemic in the United States. The Center for Disease Control and Prevention gave a retired Reeves a call to help control the outbreak. Dr. Roy Campbell, chief of the surveillance and epidemiology activity of the Arboviral Diseases Branch at the CDC had said that Reeves’s encephalitis research from a half-century earlier still provided “a roadmap for understanding West Nile virus.”
But with time comes new outbreaks—and an increasing need to deeply and widely understand the world of arthropods and the diseases they carry. The work of Reeves, Harris, and Marshall show that this understanding lies on a spectrum—from the ecology of the mosquito and where they spawn, to the deep science of what they transmit, to the communities these viruses affect. One researcher can’t do this work on his or her own. But the faculty at UC Berkeley show that one researcher can certainly do plenty.
At the end of his career, Hughes asked Reeves, “Do you look upon yourself as an entomologist, an epidemiologist, or something else?”
To which he answered with a laugh. “Yes.”